Strengthen alliances within and beyond the HIV community
The HIV care pathway is not a simple one and partnerships and collaboration are key to ensuring that it is possible to navigate a complicated system . We heard that in many instances, because budgets are limited, services operated in siloes or did not have capacity to collaborate, which led to waste and poorer care . As our healthcare system is increasingly organised around ‘patient focused’ care, it is essential that the system is easy to navigate, including between clinical and non-clinical needs . HIV is not the only long-term condition where this can be the case, and often people living with HIV experience less coordinated care because they are living with comorbidities which they are also managing.
Most of the success achieved on HIV treatment and prevention in England, has been a result of strong partnerships . They have played a key role on accelerating the country’s progress on HIV . The commission received a strong body of evidence of good practice including work among national and local government, community-based organisations, professional bodies, academia, private sector, activists and community members.
Partnerships and collaboration between stakeholders help to pool resources, share skills and experience, share best practice, ensure services are accessible and acceptable, ensure messaging is appropriate and effective, avoid competing for campaign space and prevent disjointed pathways along which the most vulnerable often are lost.
We also know partnerships do not come without challenges and there is not a single formula applicable to all . Each partnership should look into what works and what needs should be addressed . But even then, challenges remain . For example, HIV service providers including community organisations and charities operate in a competitive environment bidding against each other during the commissioning of services . In a landscape of reducing funds, this creates barriers for cooperation among organisations.
When national, regional and local level partnerships are not coordinated, there is a risk of conflicting priorities or duplication of efforts and resources . More generally, differing cultures, goals and priorities between stakeholders can hinder effective partnerships . So it is important to build strong leadership, commitment, respect, shared visions and pool resources to overcome those challenges.
Integration of care
“Poor integration of care can result in delayed or poorly-informed clinical decisions. People living with HIV lose confidence in the healthcare system and disengage. Some have died as a result.”
National AIDS Trust
HIV prevention and care is commissioned by multiple bodies and provided by national and local public, voluntary and private sector organisations . This can lead to a fragmentation of services, patients who are lost from the system when they fall out of contact and therefore do not get the healthcare they need, and the duplication of efforts . Addressing this will be even more crucial as the system manages national level changes to public health bodies and the related implications of this .
“Our experience is that the pathways between primary, secondary and
community based care need to be further developed and strengthened. Far too many people ‘fall through the net’. They remain disconnected, unwell and isolated, and ultimately have poorer health outcomes and early deaths.”
The Food Chain
Commissioning
In 2012, the Health and Social Care Act changed the structure of healthcare in England . The Act separated treatment and care from prevention and public health . Responsibility for local public health services was passed to local authorities and Public Health England was created as a national body .73 Most aspects of HIV prevention have been commissioned by local authorities since .74 This includes those prevention interventions provided within sexual health services – both clinics and online provision is now split across multiple organisations . Local NHS clinical commissioning groups (CCGs) pay for HIV testing in primary care (for example, in GPs) and in secondary care (for example, in A&E or antenatal testing) . Public Health England commissions the national HIV Prevention England programme, and the national home sampling programme that aim to complement local prevention efforts . NHS England (the national body) is responsible for commissioning HIV treatment services . Responsibility for HIV support services (which are non- clinical interventions) are locally determined.
The fragmentation of commissioning remains a significant obstacle to more effective joined-up HIV services and has become more visible over recent years . Successive cuts to the ring-fenced public health grant has led to a 25% reduction in local authority spending on sexual health services (including HIV prevention services) between 2013/14 and 2017/18, within the context of increasing demand for some services.
Cuts and changes to one body have knock on impacts for others . Changes to social support services have resulted in increased pressure on HIV treatment services to provide support with social care issues . The impact of changes to service models or the retendering of part of a service where HIV and sexual health services are integrated and share a specialised workforce, causes destabilisation of wider services, fragmentation and increased costs.
When there are disagreements on who is responsible for aspects of the HIV pathway, the impact can be serious reductions in access . An example is PrEP, where a lack of agreement on who was responsible for its commissioning resulted in National AIDS Trust taking the issue to the High Court . With regards to HIV prevention (and broader sexual health), there is an increasing movement (supported by the Department of Health and Social Care and Public Health England) for collaborative commissioning between local authorities and NHS organisations .75 All of these organisations with responsibility for commissioning aspects of the “HIV pathway” will need to play a key role in achieving the 2030 goals.
Managing complex needs
Increasingly the health and social care system in the UK is intended to focus on ‘person-centred’ care – a holistic approach where an individual’s care is organised in an integrated way, with each element of care delivered with thought to a person’s wider needs . Person-centred care puts the patient first and developing systems that can support it requires patient involvement and co-design . It is especially important for people who experience a number of healthcare needs – ‘multi-morbidity’ or ‘comorbidity’ – where, historically, care for each health condition has been planned in isolation . Those who have complex needs (medical and non-medical) are more likely to be impacted by lack of integration . Poorly integrated care can cause inconvenience and unnecessary costs, but also risks clinically poor outcomes or even potentially dangerous treatment . The solution involves healthcare based on integrated provision that is well coordinated between different healthcare providers . As the cohort of people living with HIV in the UK is ageing, multi-morbidity is increasingly an important matter in managing their treatment and care . People living with HIV tend to experience multi-morbidity at an earlier age than the general population . Distinct from the impact of ageing, for some people living with HIV the presence of non-clinical complexity, including factors such as use of social care, poverty, insecure housing, or migrant status, can also affect treatment and care needs . Difficulties in having to manage multiple appointments, with multiple consultants and providers, means that attending health appointments becomes expensive and all-consuming . Uncertainty over clinical responsibility undermines patient confidence in care . Inconsistent, sometimes contradictory, advice and treatment decisions lead to a lack of confidence in medical opinion . Having multiple tests, especially blood tests, sometimes being repeated only a few days apart, is frustrating and wasteful.
Care pathways for people living with HIV are often fragmented, affecting care for all but particularly for those with complex needs . HIV services are often unable to refer patients onto other services or referrals are not smooth, which means people are lost to follow up.
“Being able to cross-refer to other services, for example domestic violence, drug and alcohol, or even better, to work alongside these services to give wrap-around support when requested by the service user would also allow less scary and more positive conversations regarding how to make lifestyle changes as well as reducing duplication of services.”
Mary
People’s experience of living with HIV often intersects with their other needs . We know that the HIV epidemic does not exist in isolation and recognise that tackling other STIs and blood borne viruses is key to reaching our goal . Particularly in Birmingham, multiple stakeholders highlighted that hepatitis was a big issue in the city and that combined testing initiatives were necessary to tackle the two epidemics .76 We heard that testing is incredibly fragmented and happens in silos, leading to duplication or missed opportunities . We agree that pairing HIV testing with other tests is not only practical but would serve to normalise HIV testing . Recent work in Merseyside, where testing services run by Liverpool University Hospital NHS Foundation Trust tested 400 people in temporary housing (housed during the pandemic) has led to 60 people being put on treatment plans for HIV and hepatitis C .77
Partnerships working is often strongest in the community sector, where organisations build off each other’s expertise to reach new audiences and share best practice . We saw many great examples of partnership working, including in Manchester where we were hosted by the PaSH partnership; an alliance between The George House Trust, LGBT Foundation and BHA For Equality who work together on local health campaigning . The Fast Track Cities initiatives provided a space for partnership building across the sector in many cities we visited, bringing together community organisations, sexual health services, local government leadership and NHS bodies around a common goal.
It is clear that further collaboration is necessary across public health services to ensure that people do not fall through the gaps . Clinicians, support services and people living with HIV all expressed that there is a need for better collaboration with other public health services and community organisations, including but not exclusive to drug and alcohol services, mental health services and domestic violence services . This is to ensure clear referral pathways and shared knowledge.
Mental health
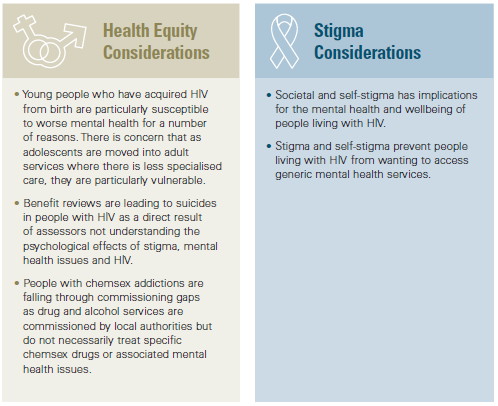
Compared with the general population, people living with HIV are twice as likely to have a mental health issue .78 While not everyone living with HIV will experience mental health issues within their lifetime, there is clear evidence to show that mental health and HIV are closely interrelated and that in order to treat HIV effectively you cannot ignore a person’s mental health . However, 40% of HIV clinics do not have access to a psychological or mental health professional within their multidisciplinary teams (MDTs) .79 In the past HIV support services have provided psychosocial support for people who are newly diagnosed or struggling to cope with their HIV diagnosis . Many of these services have been decommissioned leaving people no choice but to access generic services for their mental health needs associated with HIV diagnosis . These services are simply not as effective for people with HIV. We know that stigma around HIV is still very much alive and severely impacts on a person’s wellbeing and mental health and in extreme cases have even resulted in suicide.
Mental health support is proven to increase adherence to HIV medication by 83% in people with depression . Despite the clear public health benefits to treating mental health issues in people with HIV, it is generally not until people reach the more severe end of the mental health spectrum that specialised HIV services that support good mental health are provided.
The commissioning landscape for HIV and mental health is extremely complex because they are two separate conditions with different commissioning arrangements and pathways . While the government is committed to parity of esteem between physical and mental health, there is a lack of understanding of why generic services can often not meet the needs of people living with HIV.
“There are additional issues now where HIV services have to refer to primary care for all other ongoing health issues which means that, for
example, someone identified with depression which could be treated in the HIV services now has to go their GP who, on the whole, are not
proactive in calling patients even after letters from the clinic, so we rely upon the patient having the motivation to go to their GP to treat
their depression which, due to numerous circumstances (unable to get a timely appointment, difficult booking systems, being sent back to the HIV services) they may not do and this will not be picked up until the next HIV appointment or if the individual deteriorates. Therefore there is a lack of robust pathways to support this.”
Shaun Watson
Not only are pathways to mental health support unclear, but often generic mental health services are not equipped to support people living with HIV . People living with HIV who want to access services are concerned about stigma and confidentiality, and so often feel better supported in HIV specific services . The APPG on HIV and AIDS recently reported that the
government’s commitment to parity of esteem between physical and mental health services has brought investment in generic mental health services, but this misses this nuance that people living with HIV want prioritisation of HIV specialist mental health support, not just to access generic services .80
“When diagnosing HIV, it was felt that there was very poor support offered. Peer support or support from a counsellor or social worker should be on hand at the point of diagnosis where possible.”
Body Positive
The community sector plays a substantial role in supporting people living with HIV to navigate care and delivering prevention . This often goes unacknowledged or is not considered an important part of a care pathway . Provision of peer support – where support is provided by people living with HIV, for people living with HIV – is a key component of this, but provision is patchy as services often rely on commissioners funding support via community services . This is despite the fact that in 2018, 1 in 5 people living with HIV said that they had needed help dealing with isolation and loneliness in the last year.81 In Bristol, Brigstowe aims to have peer support available in clinic at everyone’s first appointment at the Brecon Unit in Southmeads Hospital . This gives an immediate link into support after clinical appointments . Currently, there is no clear commissioning home which assigns responsibility for providing such services, so it only occurs in some local instances . Provision must become consistent across the country.