
At the beginning of our journey as an HIV Commission, we reviewed published evidence and heard from leading HIV specialists about the current shape of the epidemic. Later, we reviewed and discussed the latest annual HIV statistics published by the HIV surveillance team at Public Health England . A team globally recognised as being first class that has provided us with data to inform our work across the year.
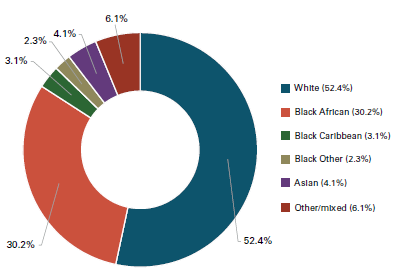
This work must be a priority for the newly created National Institute for Health Protection. The graphs below show the current data we have on HIV in the UK – who is affected and how – which served to frame our understanding and our findings. However, the data we do have falls short of what is needed . In our actions below, we highlight what data improvements we need to end new HIV transmissions by 2030 . In order for our response to be agile as new HIV transmissions fall, we need more granular data which is easily accessible to everyone . Particularly, we must better collect data on more subpopulations by unpacking the ethnic category ‘other’ to really understand who is affected by HIV (see Action 7) .
This category refers to multiple ethnic groups, so we still do not fully understand who they are and how to address their needs . Having a better understanding of who within this group are affected by HIV will be crucial to best inform the design of treatment and prevention initiatives to end new transmissions . There has been significant recent progress in HIV outcomes in England.
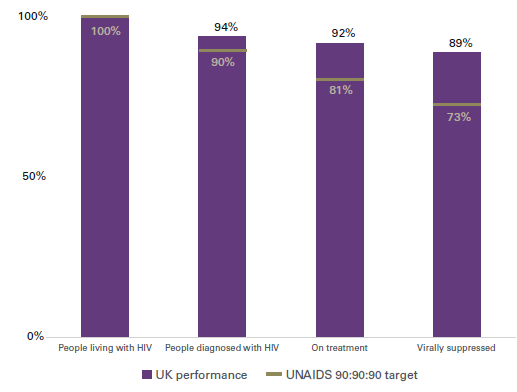
The United Nations Programme on HIV/AIDS (UNAIDS) set a series of international targets to help end the pandemic – the UNAIDS 90:90:90 targets include that:
- By 2020, 90% of all people living with HIV will know their HIV status
- By 2020, 90% of all people with diagnosed HIV infection will receive sustained antiretroviral therapy
- By 2020, 90% of all people receiving antiretroviral therapy will have viral suppression.
In England in 2019, 94% of people living with HIV have been diagnosed, 98% of those are on treatment, and of them, 97% are now ‘undetectable’ . The success shows what is possible and why complacency now would be a big mistake as we look forward to our 2030 ambition .
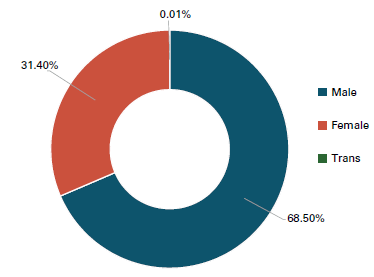
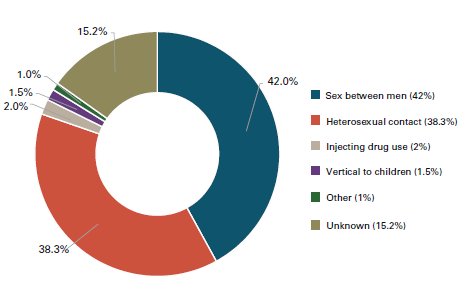
The most recent estimates suggest that in 2019 there were 96,200 people living with HIV in England . Of these, around 5,900 are undiagnosed in England – by definition they do not know they are living with HIV . Late diagnoses cause complications for the individual and risk preventable new HIV transmissions . While anyone can get HIV, some populations are disproportionately affected . In England, gay and bisexual men and Black African people continue to be the most acutely affected by HIV. We also know that London has consistently had the highest rates of HIV in the country, making up 40% of new diagnoses in 2019. Patterns of HIV transmission are not static and the people most at risk can change over time. We must be ready to respond to these changes.
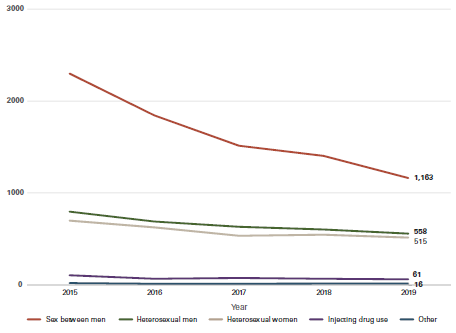
Since 2014, there has been a decline in the number of people diagnosed with HIV each year (new diagnoses) and a decline in the number of people that Public Health England estimates to have acquired HIV each year (incidence rate) . These declines have not been spread equally amongst all key population groups or across regions .1 The most significant drop has been amongst white gay and bisexual men living in London, aged 25 to 49, increasing numbers of gay and bisexual men born abroad are more likely to be diagnosed with HIV than those born in the UK.2
The number of new diagnoses each year is sometimes used as a proxy for incidence (the number of new transmissions which actually occurred) . New diagnoses and incidence rates are however different . A short-term rise in new diagnoses would occur if testing becomes routine in the health service (see Action 4) and we are able to find more of the undiagnosed people living with HIV . This would be a success not a failure. For this reason everyone serious about ending new transmissions must track our progress against estimated incidence of HIV, not new diagnoses alone.
